
The condition known as medial arcuate ligament syndrome (MALS) is characterized by excessive compression of the celiac plexus and celiac artery, two major branches of the aorta that supply blood to the stomach, liver, and other organs.
Table of Contents
What is Median Arcuate Ligament Syndrome?
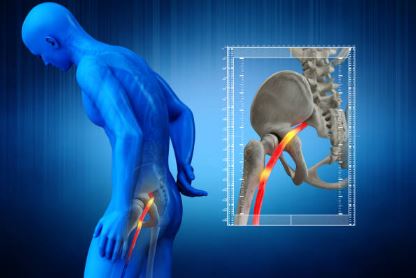
Median arcuate ligament syndrome (MALS) develops when the artery that supplies blood to the upper abdomen is compressed by the arc-shaped band of tissue in the chest region. It is known as the celiac artery. MALS can cause stomach pain in some people.
Who Median Arcuate Ligament Syndrome Occur?
Each individual has a slightly different location for the celiac artery and median arcuate ligament. Typically, the ligament crosses the aorta, the body’s largest blood vessel. The celiac artery is above it. But sometimes the ligament or artery may be out of place, causing MALS. The celiac plexus, a network of nerves that surrounds the celiac artery, may also be under pressure from the ligament.
MALS may occur in anyone, even children. Other names for MALS are:
- Celiac artery compression
- Celiac axis syndrome
- Dunbar syndrome
To release (decompress) the ligament and reestablish blood flow through the artery, surgery is used as a form of treatment.
What Are the Symptoms of Median Arcuate Ligament Syndrome?
Celiac artery compression frequently goes unnoticed.
MALS sufferers, however, may experience persistent (chronic) stomach pain over an extended period of time. The celiac artery may not be receiving enough blood flow, or nearby nerves may be being compressed, which would cause the symptoms.
Symptoms of MALS include:
- Pain in the upper middle stomach area, which may go away when leaning forward
- Stomach pain after eating, exercising, or changing body position
- Bloating
- Diarrhea
- Fear of eating food due to pain, leading to significant weight loss — usually greater than 20 pounds (9.1 kilograms)
- Nausea and vomiting
When to See a Doctor?
Stomach pain can have many different causes. Call your healthcare provider if your stomach pain doesn’t go away despite treatment at home. To pinpoint the precise cause, you’ll need a thorough physical examination and tests.
Call your provider right away if your stomach pain is severe and getting up or moving makes it worse. Seek immediate medical help if your stomach pain occurs with:
- Bloody stools
- Fever
- Nausea and vomiting that don’t go away
- Severe tenderness when you touch your belly area
- Swelling of the belly area
- Yellowing of the skin or whites of the eyes (jaundice)
Upper stomach pain and chest pain can occasionally be mistaken for one another. Heart attacks can sometimes be to blame. Get emergency help or call 911 if you have chest or upper stomach pain with or without any of the following symptoms:
- Pressure, fullness, or tightness in your chest
- The crushing or searing pain that spreads to your jaw, neck, shoulders, and one or both arms
- Pain that lasts more than a few minutes or gets worse with activity
- Shortness of breath
- Cold sweats
- Dizziness or weakness
- Nausea or vomiting
What Causes Median Arcuate Ligament Syndrome?
The celiac plexus nerves are thought to be compressed or pinched by the median arcuate ligament over the celiac artery, which is thought to be the cause of MALS. In people who have carpal tunnel syndrome, the squeezing of these nerves can result in pain in their hands that is comparable to the pain they experience. Although this theory is debatable, it is possible that the celiac artery, which supplies blood to the affected organs, is not functioning properly.
What Are the Risk Factors?
Because the cause of MALS is poorly understood, the risk factors for the syndrome are unclear. MALS has been seen in children, even twins, which might mean genetics plays a role.
Some people have developed MALS after pancreatic surgery and blunt injury to the upper stomach area.
What Are the Complications?
MALS complications include long-term pain, especially after meals. Pain can cause significant weight loss and a fear of eating. The impact of the pain and any associated depression or anxiety can be significant. MALS symptoms may be vague and can mimic other conditions. Obtaining a precise diagnosis could take some time.
How is Median Arcuate Ligament Syndrome Diagnosed?
Your doctor will review your medical history and conduct a physical examination if they suspect you may have MALS. In order to rule out less uncommon causes of your symptoms, your doctor may also order a few tests, such as imaging and blood work. These include:
- GERD, or gastroesophageal reflux disease.
- Gastritis.
- Gastroparesis.
- issues with your intestines, gallbladder, liver, pancreas, or spleen.
Your doctor might prescribe a mesenteric duplex ultrasound to check the celiac artery’s blood flow and the celiac plexus’ compression after these conditions are ruled out. A CT or MRI angiogram, which can provide a clearer image of your celiac artery and aorta, would be another beneficial imaging test.
Your records will be examined, and these actions are taken, as soon as a MALS diagnosis is suspected.
- Imaging exams (like a CT/MRI angiogram or a mesenteric ultrasound of the celiac axis) will either be ordered or repeated.
- Surgeons who specialize in vascular surgery and/or minimally invasive surgery will be your consultants.
- A pain management expert will assess you to determine whether a celiac plexus block procedure is appropriate for you. This assists in making the diagnosis and provides short-term relief from the MALS symptoms.
How is Median Arcuate Ligament Syndrome Treated?
When MALS is determined to be the cause of your symptoms, your healthcare provider will probably recommend a minimally invasive (laparoscopic/robotic) procedure to release the compression of the median arcuate ligament on the aorta. By inserting instruments through five to six tiny (roughly 1/2 inch) incisions (cuts), the surgeon can divide the nerves and separate the median arcuate ligament (neurolysis).
Most MALS patients who undergo laparoscopic surgery spend the night in the hospital afterward and start eating normally the following morning. The incisions will cause you some discomfort and pain, and you will be given painkillers to ease the suffering. The majority of MALS sufferers report that after surgery, their symptoms, such as pain when eating, have improved. Probably two weeks will pass before you can resume your regular activities.
About 10% of people with MALS have a traditional “open” operation. Your surgeon will make a significant incision down the center of the abdomen, frequently with the help of a vascular surgeon. The recovery period following this procedure could last between three and five days in the hospital. Within four to six weeks, you can usually resume your regular activities.
What Type of Follow-up Care is Needed After Surgery?
One month following surgery, duplex ultrasound is typically performed on the majority of MALS patients to ensure that the median arcuate ligament is not still being compressed. Because of the accumulation of scar tissue, the celiac artery continues to narrow in some people. Typically, this does not result in post-operative symptoms, and it is treatable non-surgically using medications or, in rare cases, another celiac plexus block. Other endovascular treatments, like celiac axis stenting, may occasionally be required.
Is MALS Syndrome Serious?
MALS complications include long-term pain, especially after meals. A fear of food and significant weight loss are two outcomes of the pain. The pain and related depression or anxiety can greatly impact the quality of life.
Is Median Arcuate Ligament Syndrome Life Threatening?
While MALS is not life-threatening, it may mimic the symptoms of mesenteric ischemia and may initially be worked up similarly in the ED, as it was in this situation.
Conclusion
A select few people with MALS who experience the condition repeatedly might be candidates for another attempt to release the scar tissue. These individuals, however, are at much higher risk (greater than 50%) of needing an open operation.